Handheld Device Puts Power of Lab-Based Diagnostic Testing in the Palm of Your Hand
July 26, 2024
Source: https://www.labmedica.com/molecular-diagnostics/articles/294801920/handheld-device-puts-power-of-lab-based-diagnostic-testing-in-the-palm-of-your-hand.html
 634
634
Many common tests for infectious diseases work by detecting either antigens related to the virus or antibodies created in response to the infection. These tests, which now include widely used COVID-19 rapid antigen tests, offer the advantages of speed and broad availability. However, polymerase chain reaction (PCR) tests still surpass these in terms of accuracy, reaching nearly 100%. PCR tests, considered the gold standard in infectious disease diagnostics, excel because they detect a pathogen’s genetic material like RNA directly. This capability increases specificity, reducing the likelihood of false positives. PCR can also amplify minimal amounts of genetic material, allowing it to detect infections at very low levels. Yet, PCR requires specialized skills and expensive equipment, which limits its availability, particularly in low-resource settings.
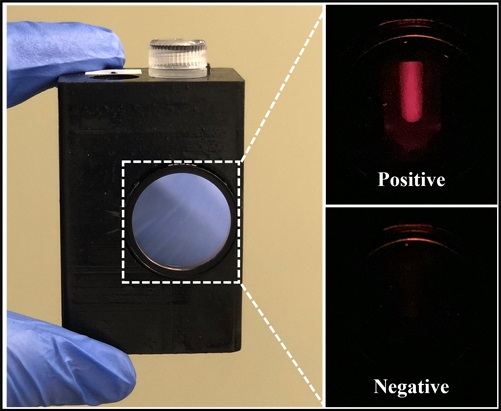
Researchers at the University of Connecticut (Storrs, CT, USA) have now developed a platform technology that incorporates PCR-like capabilities within a handheld device, as detailed in a study published in Advanced Science. This device can detect HIV and SARS-CoV-2 with PCR-level performance but is more accessible, faster, and portable, potentially making advanced diagnostics more widespread. This new device, the lab-in-a-magnetofluidic tube (LIAMT), integrates all necessary functions into a single, portable unit unlike the multiple large machines required for PCR. LIAMT simplifies the isolation of genetic material by using magnetism instead of centrifugation. It employs tiny magnetic beads within a 1.5-milliliter tube to capture viral RNA, which is then pulled through washing steps by a magnet inside the device, effectively isolating the RNA. LIAMT does not require the thermal cycling equipment typical of PCR. Instead, it uses a constant, low-temperature process facilitated by special proteins that separate and duplicate nucleic acid strands. After amplification, the LIAMT device slightly heats the sample to melt a wax barrier, releasing a solution of CRISPR enzymes that emit a fluorescent signal upon binding to their target. This signal indicates the presence of viral RNA if it's substantial enough, visible through a small window on the device.
This system, devoid of heavy equipment like centrifuges and thermal cyclers, offers a significant advancement in making diagnostic tools more accessible and faster—producing results within about an hour compared to the longer processes associated with traditional PCR, where samples often need to be sent away for analysis. To verify its effectiveness, researchers tested LIAMT against traditional PCR using swab samples for SARS-CoV-2 and blood plasma samples for HIV. The results showed LIAMT to have comparable sensitivity and specificity, aligning closely with PCR results in most cases. Encouraged by these findings, the researchers plan to further refine LIAMT’s performance and usability, particularly to enhance care for HIV patients who require regular testing. This could transform routine testing by eliminating the need for hospital visits and lengthy waits, offering instead rapid, reliable results at the point of care.
“With our device, we used the volume you could get from a finger prick to produce accurate HIV test results quickly. Patients could take these tests at a local point-of-care center or at home and receive the medication they need more quickly,” said Changchun Liu, Ph.D., a professor of biomedical engineering at the University of Connecticut.
By editor
Read more on
- Gan & Lee Pharmaceuticals’ new PROTAC drug GLR2037 tablets have been approved for clinical trials to enter the field of prostate cancer treatment March 3, 2026
- AideaPharmaceuticals plans to raise no more than 1.277 billion yuan through a private placement to focus on the global clinical development of innovative HIV drugs March 3, 2026
- Giant Exits! Its Star Business Acquired March 3, 2026
- Focusing on cardiovascular and cerebrovascular diseases! OpenMediLead Medical Intelligence Dual Engines Launch Internal Testing, Connecting Drug Development and Clinical Diagnosis in a Closed Loop March 3, 2026
- Innovent Biologics Announces Approval of New Indication for BTK Inhibitor “Pitubrutinib” in China March 3, 2026
your submission has already been received.
OK
Subscribe
Please enter a valid Email address!
Submit
The most relevant industry news & insight will be sent to you every two weeks.



