Stanford, NCI Researchers Discover New CAR-T Target With Early Study Data
November 22, 2017
Source: biospace
 909
909
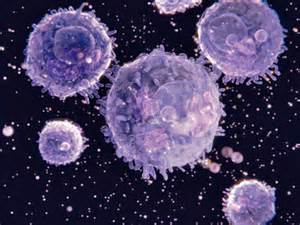
Cancer is a remarkably adaptable disease. Fast-dividing tumor cells evolve quickly to develop resistance to various drugs, as well as the new immuno-oncology approaches. CAR-T, for example, uses the body’s own immune system, engineering T-cells to identify a specific protein, CD19, on the surface of cancer cells. It’s extremely effective. However, in some patients, the cancer cells respond by no longer generating CD19 proteins, and the patient relapses or doesn’t respond to the therapy.
Researchers at Stanford University School of Medicine with the National Cancer Institute (NCI) have identified another cancer-surface molecule, CD22, and begun trials on B-cell acute lymphoblastic leukemia (ALL) patients using an immuno-oncology approach similar to CAR-T. In the Phase I trial, 15 of the 21 patients who had previously relapsed or did not respond to anti-CD19 CAR-T, were treated with an anti-CD22 CAR-T therapy. Ten of the 15 patients had already received treatment for CD19-targeted treatment.
One of six patients in the trial receiving the lowest dose achieved complete remission. At higher doses, 11 of the 15 patients, or 73 percent, went into remission. The remissions lasted a median of six months, with three remaining in complete remission at six, nine and 21 months after therapy.
“The take-home message is that we’ve found another CAR T-cell therapy that displays high-level activity in this Phase I trial,” said Crystal Mackall, associate director of Stanford’s Cancer Institute and director of the Parker Institute for Cancer Immunotherapy at Stanford, in a statement. “But the relapse rate was also high. So this forces the field to get even more sophisticated. How much of a target is needed for successful, long-lasting treatment? What happens if we target both CD19 and CD22 simultaneously?”
A trial is already under way for a CAR-T cell that recognizes CD19 and CD22. The study was published in the Nov. 20 online issue of Nature Medicine. Terry Fry, a pediatric hematologist and oncologist at the NCI is the lead author.
Researchers at Seattle Children’s initiated a similar trial only days ago in acute lymphoblastic leukemia (ALL).
“This is an exciting time when we’re at the forefront of advancing the CAR T-cell immunotherapy field by pioneering strategies to improve long-term outcomes for children and young adults,” said Rebecca Gardener, lead investigator of the PLAT-05 trial and oncologist at Seattle Children’s, in a statement. “In launching a bilateral attack on the cancer cells, we hope this trial will help us develop a T-cell therapy that leads to long-term remission for many more of our patients.”
John Carroll, writing for Endpoints News, notes, “The small trial at Stanford is significant for a variety of reasons. While Novartis and Gilead/Kite have begun the process of fielding the first new therapies, the emphasis in research circles has shifted to creating a new, safer generation of CAR-Ts that can be far more durable. Also, Mackall told The New York Times, it’s important to understand that CD19, for all its remarkable effect in offering a beacon for cell therapies, is ‘not some kind of unicorn.’”
By DduRead more on
- Things to Know before Buying Newborn Baby Incubators March 31, 2022
- CRUK researchers develop new early-stage rectal cancer treatment December 12, 2020
- Highly Resistant Food Poisoning Bug Responds to Antibiotics September 6, 2018
- Smartphone Based Diagnosis to Identify Mosquitoes Transmitting Infection September 5, 2018
- 3 Natural Plant Extracts Manufacturers on Drugdu.com September 4, 2018
your submission has already been received.
OK
Subscribe
Please enter a valid Email address!
Submit
The most relevant industry news & insight will be sent to you every two weeks.



