New Synthetic Biomarker Technology Differentiates Between Prior Zika and Dengue Infections
May 16, 2024
Source: drugdu
 312
312
 Until now, researchers and clinicians have lacked diagnostic tools to easily differentiate between past infections with different flaviviruses—a family of mostly mosquito- and tick-borne viruses that include Zika and dengue. This challenge has hindered clinical-epidemiologic studies, viral diagnostics, and vaccine development. Antibodies for Zika virus, a mosquito-borne virus that spread to the Americas in 2015 and continues to cause sporadic outbreaks, can often be mistaken for dengue virus antibodies in many diagnostic tests. This confusion makes it difficult to determine if a person who tests positive had dengue, Zika, or both. For reproductive-age women, it is particularly crucial to know if they have had Zika and likely have immunity since infection during pregnancy can lead to birth defects. Knowing their immunity status can guide their efforts to avoid mosquito bites in endemic areas during pregnancy. Now, a newly discovered Zika virus-specific synthetic molecule can distinguish Zika-immune patient samples from those previously infected with dengue virus. This technology may lead to the development of better diagnostics and vaccine candidates.
Until now, researchers and clinicians have lacked diagnostic tools to easily differentiate between past infections with different flaviviruses—a family of mostly mosquito- and tick-borne viruses that include Zika and dengue. This challenge has hindered clinical-epidemiologic studies, viral diagnostics, and vaccine development. Antibodies for Zika virus, a mosquito-borne virus that spread to the Americas in 2015 and continues to cause sporadic outbreaks, can often be mistaken for dengue virus antibodies in many diagnostic tests. This confusion makes it difficult to determine if a person who tests positive had dengue, Zika, or both. For reproductive-age women, it is particularly crucial to know if they have had Zika and likely have immunity since infection during pregnancy can lead to birth defects. Knowing their immunity status can guide their efforts to avoid mosquito bites in endemic areas during pregnancy. Now, a newly discovered Zika virus-specific synthetic molecule can distinguish Zika-immune patient samples from those previously infected with dengue virus. This technology may lead to the development of better diagnostics and vaccine candidates.
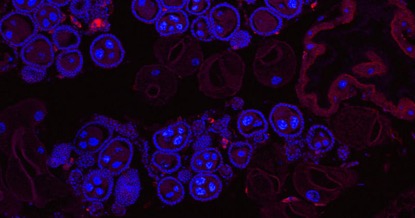
The study, led by researchers at the University of Pittsburgh (Pittsburgh, PA, USA) and The Herbert Wertheim UF Scripps Institute for Biomedical Innovation & Technology (Jupiter, FL, USA), is the first to apply the novel “epitope surrogate” technology to Zika. The research team utilized an approach pioneered by co-senior author Thomas Kodadek, Ph.D., a chemist with The Wertheim UF Scripps Institute, to screen half a million “peptide-inspired conformationally constrained oligomers,” or PICCOs, against blood samples from individuals infected with either dengue or Zika virus. PICCOs are nonorganic molecular shapes attached to microscopic plastic beads that mimic epitopes—the parts of a pathogen that an antibody would bind to in order to neutralize the threat.
If any of the PICCOs match the shape of an antibody in the blood sample, the antibody will bind to them, allowing researchers to "fish" it out. The presence of an antibody against a virus in a person's blood indicates a past infection or vaccination, prompting the immune system to produce antibodies. The researchers identified 40 PICCOs that interacted with Zika virus antibodies. After screening these against dengue-positive blood, one PICCO, named CZV1-1, was particularly effective at binding Zika antibodies but not dengue antibodies. This single CZV1-1 PICCO synthetic molecule correctly identified individuals previously infected with Zika virus 85.3% of the time and produced false positives in only 1.6% of tests, rates comparable to COVID-19 antibody tests. Notably, the PICCO screening technology used to identify the Zika-specific molecule does not require refrigeration and could also be adapted for other outbreaks.
“The technology is amazing. You don’t need to know the sequence, or the structure, or even the pathogen,” said co-senior author Donald Burke, M.D., Pitt Public Health dean emeritus. “As long as you have chosen the right sets of patient blood samples to compare, you can tease out the important antibodies that differ between the patient sets, along with the corresponding synthetic molecule biomarkers.”
Source:
https://www.labmedica.com/molecular-diagnostics/articles/294801144/new-synthetic-biomarker-technology-differentiates-between-prior-zika-and-dengue-infections.html
Read more on
- Gusekirumab Injection Accepted by CDE, Multiple Pipelines Advancing Simultaneously March 4, 2026
- Yifan Pharmaceutical’s teriparatide injection has been accepted by the CDE (Center for Drug Evaluation), adding a new domestic player to the osteoporosis treatment field March 4, 2026
- //news.yaozh.com/archive/47318.html PD-1 sales surge March 4, 2026
- A major breakthrough! Roche’s oral BTK inhibitor achieves its third Phase III clinical trial victory, a game-changer in the multi-billion dollar MS (manufactured pharmaceuticals) market. March 4, 2026
- GB19 Injection Approved for Clinical Trials of Cutaneous Lupus Erythematosus March 4, 2026
your submission has already been received.
OK
Subscribe
Please enter a valid Email address!
Submit
The most relevant industry news & insight will be sent to you every two weeks.



