Machine Learning Model Calculates Chemotherapy Success in Patients with Bone Cancer
January 6, 2024
Source: drugdu
 373
373
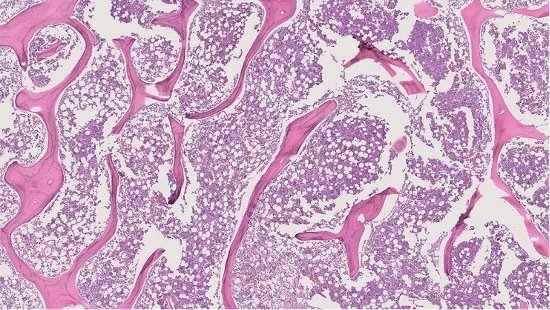 The calculation of Percent Necrosis (PN) — the proportion of a tumor considered inactive or "dead" following chemotherapy — serves as a vital predictor of survival outcomes in osteosarcoma, a type of bone cancer. For instance, a PN of 99% signifies that 99% that the tumor is dead, indicating the patient's positive response to chemotherapy and potentially better survival prospects. Pathologists typically assess PN by meticulously examining, interpreting, and marking up whole-slide images (WSIs), which are detailed cross-sections of specimens (like bone tissue) prepared for microscopic examination. Nevertheless, this traditional method is not only time-consuming and demands specialized expertise but also suffers from significant variability among observers. This means two pathologists might report differing PN estimates from the same WSI. Now, a machine learning model created and trained to calculate PN has shown that its calculation was 85% correct when compared to the results of a musculoskeletal pathologist, with the accuracy improving to 99% upon excluding an outlier.
The calculation of Percent Necrosis (PN) — the proportion of a tumor considered inactive or "dead" following chemotherapy — serves as a vital predictor of survival outcomes in osteosarcoma, a type of bone cancer. For instance, a PN of 99% signifies that 99% that the tumor is dead, indicating the patient's positive response to chemotherapy and potentially better survival prospects. Pathologists typically assess PN by meticulously examining, interpreting, and marking up whole-slide images (WSIs), which are detailed cross-sections of specimens (like bone tissue) prepared for microscopic examination. Nevertheless, this traditional method is not only time-consuming and demands specialized expertise but also suffers from significant variability among observers. This means two pathologists might report differing PN estimates from the same WSI. Now, a machine learning model created and trained to calculate PN has shown that its calculation was 85% correct when compared to the results of a musculoskeletal pathologist, with the accuracy improving to 99% upon excluding an outlier.
A research team at Johns Hopkins Medicine (Baltimore, MD, USA) is developing a "weakly supervised" machine learning model, one that doesn't require extensive annotated data for training. By doing so, a pathologist would only need to provide partially annotated WSIs, significantly easing their workload. To develop the machine learning model, the team began by collecting WSIs from patients with intramedullary osteosarcoma (originating within the bone) treated with chemotherapy and surgery between 2011 to 2021. A musculoskeletal pathologist then partially labeled three tissue types on these WSIs: active tumor, dead tumor, and non-tumor tissue and also provided a PN estimate for each case. This data formed the foundation for the model's training.
The model was trained to recognize and categorize image patterns. The WSIs were segregated into thousands of smaller patches, divided into groups as per the pathologist's labels, and then fed into the model. This process aimed to provide the model a more robust frame of reference rather than just feeding it one large WSI. Upon completion of the training, the model was tested alongside the musculoskeletal pathologist on six WSIs from two patients. The results demonstrated an 85% correlation in PN calculations and tissue labeling between the model and the pathologist. However, the model struggled to accurately label cartilage, leading to an outlier as a result of an abundance of cartilage on one WSI. When this outlier was removed, the correlation soared to 99%. Future work will focus on incorporating cartilage tissue in the model's training and broadening the WSIs range to encompass various osteosarcoma types, not just intramedullary.
“If this model were to be validated and produced, it could help expedite the evaluation of chemotherapy’s effectiveness on a patient — and thus, get them a prognosis estimate sooner,” said Christa LiBrizzi, M.D., co-first author of the study and a resident with Johns Hopkins Medicine’s Department of Orthopedic Surgery. “That would reduce health care costs, as well as labor burdens on musculoskeletal pathologists.”
Source:
https://www.labmedica.com/pathology/articles/294799814/machine-learning-model-calculates-chemotherapy-success-in-patients-with-bone-cancer.html
Read more on
- The first subject has been dosed in the Phase I clinical trial of Yuandong Bio’s EP-0210 monoclonal antibody injection. February 10, 2026
- Clinical trial of recombinant herpes zoster ZFA01 adjuvant vaccine (CHO cells) approved February 10, 2026
- Heyu Pharmaceuticals’ FGFR4 inhibitor ipagoglottinib has received Fast Track designation from the FDA for the treatment of advanced HCC patients with FGF19 overexpression who have been treated with ICIs and mTKIs. February 10, 2026
- Sanofi’s “Rilzabrutinib” has been recognized as a Breakthrough Therapy in the United States and an Orphan Drug in Japan, and has applied for marketing approval in China. February 10, 2026
- Domestically developed blockbuster ADC approved for new indication February 10, 2026
your submission has already been received.
OK
Subscribe
Please enter a valid Email address!
Submit
The most relevant industry news & insight will be sent to you every two weeks.



