Fluid Biomarker Test Detects Neurodegenerative Diseases Before Symptoms Appear
March 28, 2024
Source: drugdu
 353
353
 Amyotrophic lateral sclerosis (ALS, also known as Lou Gehrig’s disease) and frontotemporal dementia (FTD) are two progressively neurodegenerative conditions that damage essential nerve cells. ALS compromises nerve cells in the brain and spinal cord, leading to movement impairment, while FTD damages brain areas responsible for personality, behavior, and language. Studies indicate that in ALS or FTD patients, TAR DNA-binding protein 43 (TDP-43) malfunctions. This disruption prevents the correct splicing of ribonucleic acid (RNA), essential for generating proteins necessary for nerve growth and function. Instead, RNA strands become riddled with erroneous code sequences, known as "cryptic exons," which are linked to an elevated risk of developing ALS and FTD. The timing of this anomaly in the disease progression of ALS and FTD was previously unknown.
Amyotrophic lateral sclerosis (ALS, also known as Lou Gehrig’s disease) and frontotemporal dementia (FTD) are two progressively neurodegenerative conditions that damage essential nerve cells. ALS compromises nerve cells in the brain and spinal cord, leading to movement impairment, while FTD damages brain areas responsible for personality, behavior, and language. Studies indicate that in ALS or FTD patients, TAR DNA-binding protein 43 (TDP-43) malfunctions. This disruption prevents the correct splicing of ribonucleic acid (RNA), essential for generating proteins necessary for nerve growth and function. Instead, RNA strands become riddled with erroneous code sequences, known as "cryptic exons," which are linked to an elevated risk of developing ALS and FTD. The timing of this anomaly in the disease progression of ALS and FTD was previously unknown.
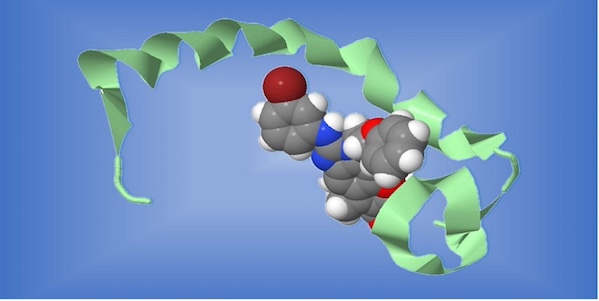
Now, researchers from Johns Hopkins Medicine (Baltimore, MD, USA) have developed a method for identifying a specific protein, hepatoma-derived growth factor-like 2 [HDGFL2], linked to TDP-43 dysfunction. Identifying this protein has led to a biomarker that could detect ALS and FTD at their initial stages, possibly before symptoms manifest. The search began with identifying cryptic exon-linked proteins related to TDP-43 function loss, followed by utilizing fragments from those proteins known as cryptic peptides for creating monoclonal (laboratory-made) antibodies specific to each one. These antibodies, when introduced into blood or cerebrospinal fluid samples, bind exclusively to their target cryptic peptides for which they were designed, enabling protein detection.
The team validated this method using blood and cerebrospinal fluid samples from three different groups, including people with the most common forms of familial (genetic) ALS and FTD linked to a mutation in the C9orf72 gene, sporadic (not defined as genetic) forms of ALS and FTD, and healthy controls. They also tested biofluid samples from pre-diagnostic stages, meaning that the researchers could look for cryptic HDGFL2 at both presymptomatic and symptomatic stages of the diseases. The test successfully identified cryptic HDGFL2 in early disease phases in genetically predisposed individuals who were expected to go on to develop the diseases, suggesting its potential as a preclinical biomarker for ALS and FTD risk prediction.
Furthermore, the test detected higher levels of cryptic HDGFL2 in fluids of individuals with sporadic ALS and FTD, underscoring the biomarker's capability to identify the disease in the absence of a known family history. By detecting cryptic HDGFL2 in presymptomatic stages, researchers can compare its effectiveness with an established biomarker for ALS and FTD. The team is now expanding its sample pool globally to validate the effectiveness, reliability, and sensitivity of their biomarker. They aim to use it as a clinical tool and to assess therapy effectiveness in ALS and FTD by monitoring changes in cryptic HDGFL2 levels and restoration of TDP-43 functionality post-treatment.
“Of all the cryptic peptides for which we made monoclonal antibodies, the one that worked best was the one designed for the cryptic HDGFL2 protein,” said Katie Irwin, an M.D./Ph.D. student at the Johns Hopkins University School of Medicine. “We used that monoclonal antibody to develop an extremely sensitive detection test for the cryptic HDGFL2 protein in body fluids.”
Source:
https://www.labmedica.com/molecular-diagnostics/articles/294800658/fluid-biomarker-test-detects-neurodegenerative-diseases-before-symptoms-appear.html
Read more on
- Gusekirumab Injection Accepted by CDE, Multiple Pipelines Advancing Simultaneously March 4, 2026
- Yifan Pharmaceutical’s teriparatide injection has been accepted by the CDE (Center for Drug Evaluation), adding a new domestic player to the osteoporosis treatment field March 4, 2026
- //news.yaozh.com/archive/47318.html PD-1 sales surge March 4, 2026
- A major breakthrough! Roche’s oral BTK inhibitor achieves its third Phase III clinical trial victory, a game-changer in the multi-billion dollar MS (manufactured pharmaceuticals) market. March 4, 2026
- GB19 Injection Approved for Clinical Trials of Cutaneous Lupus Erythematosus March 4, 2026
your submission has already been received.
OK
Subscribe
Please enter a valid Email address!
Submit
The most relevant industry news & insight will be sent to you every two weeks.



