Chip Monitors Cancer Cells in Blood Samples to Assess Treatment Effectiveness
February 1, 2024
Source: drugdu
 532
532
 Approximately only half of cancer patients see a positive response to treatments, with the remaining experiencing inadequate outcomes. The high costs and potential adverse reactions of treatments make it crucial for clinicians to quickly determine their effectiveness, or if an alternative therapy is more suitable. Presently, it can take weeks or months to fully gauge the success of cancer treatment, typically using CT scans to measure significant size changes in tumors. While tumor biopsies offer more precise data, their infrequency limits the ability to provide ongoing updates. As a solution, many clinicians are now resorting to liquid biopsies, which involve testing for cancer indicators in a patient's blood, like tumor-shed cancer cells. However, these tests require sufficiently high cell levels for detection. This is particularly challenging in lung cancer, where some FDA-approved methods for detecting blood-borne cancer cells are ineffective, often due to targeting a single, less common protein in lung cancers.
Approximately only half of cancer patients see a positive response to treatments, with the remaining experiencing inadequate outcomes. The high costs and potential adverse reactions of treatments make it crucial for clinicians to quickly determine their effectiveness, or if an alternative therapy is more suitable. Presently, it can take weeks or months to fully gauge the success of cancer treatment, typically using CT scans to measure significant size changes in tumors. While tumor biopsies offer more precise data, their infrequency limits the ability to provide ongoing updates. As a solution, many clinicians are now resorting to liquid biopsies, which involve testing for cancer indicators in a patient's blood, like tumor-shed cancer cells. However, these tests require sufficiently high cell levels for detection. This is particularly challenging in lung cancer, where some FDA-approved methods for detecting blood-borne cancer cells are ineffective, often due to targeting a single, less common protein in lung cancers.
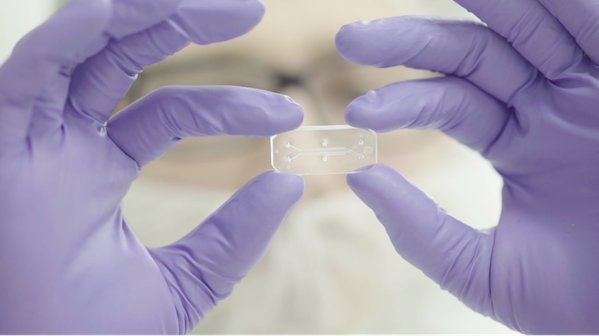
A breakthrough device now enables the determination of treatment efficacy within as early as four weeks by isolating minimal numbers of cancer cells from blood samples. Utilizing a chip to process these samples, doctors can track the quantity of cancer cells in a patient's blood to assess treatment effectiveness within the first month. This technology, known as the "GO chip," developed at the University of Michigan (Ann Arbor, MI, USA), excels where others have failed. It efficiently captures cancer cells using antibodies attached to graphene oxide sheets within the chip. These antibodies recognize a broad spectrum of cancer-specific proteins on cell surfaces. As blood flows through the chip's channels, the antibodies trap the cells, concentrating them for analysis. This not only allows for cell counting but also confirms their cancerous nature and tracks biochemical variations across patients and treatment phases.
The GO chip's capability to monitor lung cancer treatments was evaluated with 26 stage 3 lung cancer patients undergoing chemotherapy and immunotherapy. Samples were taken before treatment and after the first, fourth, 10th, 18th, and 30th weeks. The study discovered that a less than 75% reduction in blood cancer cell count by the fourth week indicated a higher likelihood of cancer persistence post-treatment. Additionally, it was observed that cancer cells from patients unresponsive to treatment exhibited activated genes potentially contributing to the cancer's resilience. These genes could be potential targets for future therapies, though more research is needed to explore this hypothesis.
“This technique has the potential to shift cancer diagnostics, moving from a delayed single assessment to a more continuous surveillance and facilitating the delivery of personalized cancer treatment,” said Shruti Jolly, professor of radiation oncology, associate chair of community practices at U-M and co-corresponding author of the study.
Source:
https://www.labmedica.com/immunology/articles/294800076/chip-monitors-cancer-cells-in-blood-samples-to-assess-treatment-effectiveness.html
Read more on
- Gusekirumab Injection Accepted by CDE, Multiple Pipelines Advancing Simultaneously March 4, 2026
- Yifan Pharmaceutical’s teriparatide injection has been accepted by the CDE (Center for Drug Evaluation), adding a new domestic player to the osteoporosis treatment field March 4, 2026
- //news.yaozh.com/archive/47318.html PD-1 sales surge March 4, 2026
- A major breakthrough! Roche’s oral BTK inhibitor achieves its third Phase III clinical trial victory, a game-changer in the multi-billion dollar MS (manufactured pharmaceuticals) market. March 4, 2026
- GB19 Injection Approved for Clinical Trials of Cutaneous Lupus Erythematosus March 4, 2026
your submission has already been received.
OK
Subscribe
Please enter a valid Email address!
Submit
The most relevant industry news & insight will be sent to you every two weeks.



