Cell Stem Cell | Drug Sensitivity and Resistance Atlas of Sarcoma
October 23, 2024
Source: drugdu
 213
213
Writing | My Best Friend Old Red Riding Hood
Sarcoma is a rare heterogeneous stromal tumor. They mainly occur in bones and soft tissues, and have a particularly severe impact on young patients [1-3]. In the United States, about 13000 cases of soft tissue sarcoma and 4000 cases of osteosarcoma are diagnosed every year. Although the incidence rate is very low, the mortality rate is still high. For example, osteosarcoma is the third leading cause of cancer death in patients under the age of 20. The treatment plan varies depending on the subtype and stage of the disease, including surgical resection, chemotherapy, targeted systemic therapy, and in some cases, radiation therapy [4,5]. Although significant progress has been made in specific subtypes, current treatment methods rarely cure them. The overall 5-year survival rate for soft tissue sarcoma is 65%, and the overall 5-year survival rate for bone cancer is 50% -60% [6].
The heterogeneity of sarcoma is manifested in over 100 different subtypes, thus the diagnosis of sarcoma also exhibits diversity: for example, it has been reported that there are 9 different subtypes of osteosarcoma [7]. About a quarter of sarcoma cases are caused by specific chromosomal fusions, such as Ewing's sarcoma, synovial sarcoma, infantile fibrosarcoma, and rhabdomyosarcoma (RMS). The genetic triggers of other bone and soft tissue sarcomas also include affecting cell cycle regulation, growth factor signaling, and angiogenesis. Specific high prevalence mutations include RTK driver mutations in epithelioid sarcoma, CDK aberrations in liposarcoma, PI3K mutations in perivascular cell tumors (PEComa) and mucinous liposarcoma. Other types of tumors, such as osteosarcoma and undifferentiated sarcoma, are complex nuclear tumors that can carry multiple mutations without a single, clear driving factor. This enormous heterogeneity increases the difficulty of determining effective treatment options for rare and ultra rare cancers, and leads to sustained low survival rates.
Precision medicine methods, as tools for identifying actionable features and improving the prognosis of each patient, are receiving increasing attention from the academic community. New generation sequencing (NGS) and immunohistochemistry technologies are widely used to identify molecular level changes and potential drug targets in patients. In the case of fusion positive sarcoma, most abnormal oncogenes cannot be directly targeted for intervention, except for NTRK. A recent study on over 6000 cases of bone and soft tissue sarcoma found that an average of 42% of tumors contained modifiable mutations. However, in multiple clinical trials over the past decade, few sarcoma patients have shown clinical benefits when using genomic precision medicine selected drugs for treatment.
Due to this genetic diversity and the limited efficacy of chemotherapy and targeted drugs selected through traditional or precision medicine, there is an urgent need to identify alternative methods to systematically evaluate the drug sensitivity and resistance of sarcomas and determine personalized treatment plans.
Recently, Alice Soragni's research group from the University of California, Los Angeles published an article titled "The Landscape of Drug Sensitivity and Resistance in Sarcoma" in Cell Stem Cell. They collected over 120 patient samples and constructed tumor organoids to study drug sensitivity and resistance in 21 types of sarcoma.
Patient derived tumor organoids (PDTOs) can simulate the behavioral characteristics of a range of malignant tumors. For various types of epithelial cancer patients, PDTOs are easy to operate and can predict body response and drug efficacy. However, the development of PDTOs for sarcoma is currently lagging behind and their application is limited.
The author used PDTOs to characterize the drug resistance and sensitivity of sarcoma. The author obtained n=194 specimens from 126 patients who underwent biopsy or surgical resection at UCLA Health Hospital, and successfully generated PDTOs from over 121 samples of primary, recurrent, and metastatic bone and soft tissue sarcoma, covering 24 different subtypes of sarcoma.
Subsequently, the author used a high-throughput organoid screening platform and combined it with histopathological testing to test the sensitivity and resistance of organoids to single and combination drugs, and obtained results within one week after surgery. The author found that drug sensitivity is related to clinical characteristics such as tumor subtype, treatment history, and disease development trajectory. PDTO screening is beneficial for optimal drug selection and can reflect the prognosis of sarcoma patients. The above work of the author can identify at least one effective treatment plan that has been approved by FDA or recommended by NCCN for 59% of the corresponding patients in the sample, which also indicates that the patient organoid based work platform developed by the author has strong clinical potential.
In summary, the author used PDTOs to detect and explore drug sensitivity and resistance patterns in 24 types of sarcoma, and found subtype specific responses in patients that are correlated with clinical features and prognosis. The author has identified actionable dosing regimens for the majority of patients corresponding to the sample, which emphasizes the enormous potential of organoids in precision medicine applications.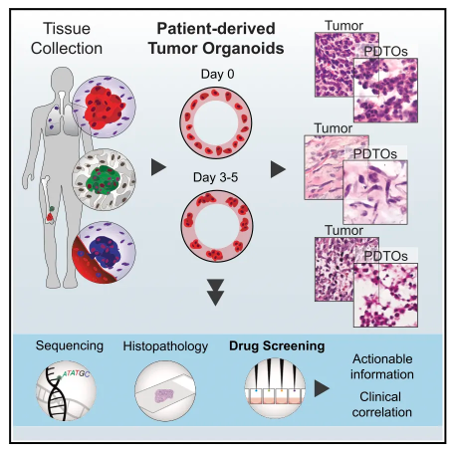
Read more on
- Gan & Lee Pharmaceuticals’ new PROTAC drug GLR2037 tablets have been approved for clinical trials to enter the field of prostate cancer treatment March 3, 2026
- AideaPharmaceuticals plans to raise no more than 1.277 billion yuan through a private placement to focus on the global clinical development of innovative HIV drugs March 3, 2026
- Giant Exits! Its Star Business Acquired March 3, 2026
- Focusing on cardiovascular and cerebrovascular diseases! OpenMediLead Medical Intelligence Dual Engines Launch Internal Testing, Connecting Drug Development and Clinical Diagnosis in a Closed Loop March 3, 2026
- Innovent Biologics Announces Approval of New Indication for BTK Inhibitor “Pitubrutinib” in China March 3, 2026
your submission has already been received.
OK
Subscribe
Please enter a valid Email address!
Submit
The most relevant industry news & insight will be sent to you every two weeks.



