the wind rises, accelerates, and accelerates again
November 1, 2024
Source: drugdu
 294
294
 The development story of tumor drugs is always so similar: the early stage may be endless suffering, but after countless failures and dashed hopes, once there is a breakthrough, the progress is often unexpected. This is the development of drugs for the treatment of small cell carcinoma (SCLC). SCLC was first discovered about 100 years ago, but it was not until 1968 that the medical community discovered its neuroendocrine origin and finally clearly distinguished it from other lung cancers.
The development story of tumor drugs is always so similar: the early stage may be endless suffering, but after countless failures and dashed hopes, once there is a breakthrough, the progress is often unexpected. This is the development of drugs for the treatment of small cell carcinoma (SCLC). SCLC was first discovered about 100 years ago, but it was not until 1968 that the medical community discovered its neuroendocrine origin and finally clearly distinguished it from other lung cancers.
In the 1980s, the treatment of platinum-containing chemotherapy combined with chest radiotherapy gradually became clear and became the basic treatment for small cell lung cancer. Although the combination of etoposide and carboplatin/cisplatin (EP) has been the standard treatment for SCLC until now; but we can also clearly see that the battle against small cell lung cancer has entered an accelerated stage. In May of this year, Amgen's DLL3/CD3 dual antibody Tarlatamab was approved, providing a new treatment option for patients with extensive-stage small cell lung cancer (ES-SCLC), sounding the battle horn. On October 24, Zai Lab released data on its DLL3 ADC drug ZL-1310 for extensive-stage small cell lung cancer. The positive clinical data results accelerated the battle against small cell lung cancer and entered a new round of "climax".
What drives global pharmaceutical companies to accelerate the battle against small cell lung cancer is the expectations of patients. For SCLC patients, chemotherapy alone is far from enough. Small cell lung cancer is very sensitive to initial radiotherapy and chemotherapy, but it is easy to develop drug resistance, and most patients will eventually die from disease recurrence. According to the stage of disease development, small cell lung cancer can be divided into limited-stage (LS-SCLC) and extensive-stage (ES-SCLC), accounting for about 1/3 and 2/3 of small cell lung cancer, respectively. The five-year survival rate of small cell lung cancer is only 7%, of which the five-year survival rate of extensive-stage SCLC is only 3% .
It is precisely for this reason that global pharmaceutical companies have invested heavily in this field, and eventually atezolizumab, Tarlatamab and other therapies have become one of the first-line and second-line treatment options for extensive-stage small cell lung cancer.
But for now, the battle against extensive-stage small cell carcinoma is far from over. There is still room for improvement in the first-line therapy. Based on overseas studies, after EP combined with immunotherapy, the improvement in OS is about 2 to 3 months, and the ORR can only be slightly improved; at the same time, the safety of treatment still needs to be improved. Because chemotherapy itself is highly toxic, PD-(L)1 combined with chemotherapy also has this problem. It is normal for the proportion of treatment-related adverse events of grade 3 or higher to be greater than 60%.
For this reason, first-line treatment of extensive-stage small cell carcinoma needs to continue to break through. And the subsequent second-line treatment is even more so. Although Tarlatamab was approved in the United States this year for the treatment of 2L+ ES-SCLC, providing patients with a new treatment option, there is still a lot of room for improvement in terms of efficacy, safety and convenience of administration. Tarlatamab's objective response rate (ORR) in the phase II clinical trial called DeLLphi-301 was relatively limited, at 40%, which means that a considerable number of patients cannot respond effectively. Moreover, among the patients who responded, the depth of remission was also limited, with a complete remission (CR) rate of only 1%.
At the same time, safety issues are a topic that Tarlatamab cannot avoid. Due to the particularity of its mechanism, Tarlatamab has side effects including severe or fatal cytokine release syndrome (CRS) and neurotoxicity. The rate of treatment-emergent adverse events (TEAEs) of grade 3 or above was as high as nearly 60%; 49% of patients experienced cytokine release syndrome (CRS), of which 26% were severe, and 7% experienced immune effector cell-associated neurotoxicity (ICANs). These side effects will not only limit its use in second-line treatment indications, but also limit its exploration in first-line treatment of SCLC. In addition, the administration of Tarlatamab is very inconvenient. Due to the existence of CRS problems, Tarlatamab adopts a recommended escalating dose regimen, which not only requires specific infusion time and infusion rate, but also requires the use of a programmable, lockable, non-elastic infusion pump equipped with an alarm.
In addition, patients need to stay in the medical center for at least one hour after the first dose for monitoring to ensure that the side effects will not endanger the patient's life [4]. Because the administration process is cumbersome, even for large cancer centers, patients need to be hospitalized, and community doctors in the United States have some difficulties in using Tarlatamab. Overall, whether it is first-line or second-line treatment, patients with extensive-stage SCLC need more and more effective therapies.
Redefining the treatment pattern of extensive-stage SCLC is still a new topic, and the huge imagination space still attracts a few adventurers around the world to move forward. In the relatively motivated domestic field, the candidate lineup that can run out has begun to surface, and the ZL-1310 mentioned above seems to have this potential. On October 24, at the 2024 EORTC-NCI-AACR (ENA) conference held in Barcelona, Spain, Zai Lab announced the global Phase 1a clinical study data of ZL-1310 in the form of an oral report at the plenary session. In terms of efficacy, ZL-1310 is extremely amazing. Phase 1a clinical study data showed that ZL-1310 showed anti-tumor activity at all dose levels, with an ORR of 74%.
In simple comparison, the response rate of ZL-1310 is not only much higher than that of Tarlatamab, but also has advantages over potential competitors. All patients included in ZL-1310 had progressed after receiving standard platinum-containing chemotherapy, 92% of patients had progressed after receiving immune checkpoint inhibitors, and 56% of patients had previously received at least two treatments but failed, that is, most of them were terminal patients with almost no drugs available. In this context, ZL-1310 can come up with more impressive data, which is undoubtedly worth looking forward to.
At the same time, several small details leave more room for imagination. First, the 74% ORR is based on all dose-escalation cohorts. If a certain medium or high dose is selected in subsequent clinical trials, the response rate may be improved. Second, ZL-1310 has excellent ability to penetrate the blood-brain barrier. Data show that up to 50% of SCLC patients will develop brain metastases during the course of the disease. Therefore, the core of a promising therapeutic drug is to have excellent ability to penetrate the blood-brain barrier. ZL-1310 targeted 6 patients with baseline brain metastases and evaluable effects, with an ORR of 100% (all of whom achieved partial remission), indicating the possibility that it could cover more patients. The currently approved indications of Tarlatamab exclude patients with symptomatic brain metastases. Third, one patient who progressed after receiving Tarlatamab treatment achieved partial remission at the time of the first tumor assessment. Although there are few cases and it cannot be proved whether it is an individual case, there is still a point of concern: while competing with Tarlatamab, ZL-1310 may also complement Tarlatamab and become a treatment option for the latter's drug-resistant group.
In addition to efficacy, another core of ZL-1310 that has attracted market attention is its outstanding safety. Whether extensive-stage small cell carcinoma tumor drugs have a higher prospect depends on two points: whether they can achieve a transition from second-line therapy to first-line therapy, and whether they can be combined with other therapies to achieve better results. The key to achieving these two drugs is that the safety is good enough. Tarlatamab has been criticized for its safety issues, and the market is worried that it will be difficult to expand its subsequent indications.
The safety advantage of ZL-1310 is more prominent: not only did no CRS and ICANS occur in the presence of dual antibodies, 20% of patients had TRAEs of grade 3 or above, and the proportion of TEAEs of grade 3 or above was 40%, but no patient terminated treatment due to TEAEs. Compared with other drugs, ZL-1310 has obvious safety advantages. As mentioned above, Tarlatamab's treatment-emergent adverse events (TEAEs) of grade 3 or above were as high as nearly 60%. Therefore, based on the current safety data, the roadmap for ZL-1310 to advance to first-line combination therapy has become clearer, which makes the future potential of this product may far exceed what is currently reflected.
In addition, ZL-1310 has been reported in both China and the United States since Phase 1. Compared with other domestic molecules, the international route is clearer and the data is more solid. Therefore, with the release of positive clinical data, some market participants believe that ZL-1310 has the potential to redefine the SCLC treatment landscape. This is also reflected in the expectations of the capital market: after the release of clinical data, Zai Lab's US stocks rose 14.65%, and Hong Kong stocks rose 15.02%.
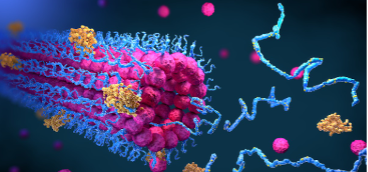
Although it is only Phase 1a clinical research data, it is not surprising that the market has high hopes for ZL-1310. On the one hand, as an important subtype of lung cancer, the patient population of small cell carcinoma is not small. Small cell lung cancer accounts for about 15% of lung cancer. Considering that lung cancer is the world's largest cancer, there are about 160,000 new small cell lung cancer patients in China each year, and nearly 400,000 patients worldwide. In view of the urgent clinical needs, the market for small cell carcinoma drugs is relatively considerable. On the other hand, ZL-1310 has the potential to cover most SCLC patients. Delta-like ligand 3 (DLL3), as a member of the Notch ligand family, is a transmembrane protein attached to the cell surface. Studies have found that DLL3 is rarely expressed in normal cells, but abnormally expressed in more than 85% of small cell lung cancers. This means that DLL3 is not only an excellent drug target, but also covers a considerable population.
For this reason, the market has always placed high hopes on DLL3 targeted drugs in the field of small cell carcinoma. In 2016, AbbVie even acquired Stemcentrx with a down payment of up to $5.8 billion and a milestone payment of $4 billion, and obtained the latter's ADC drug Rova-T targeting the DLL3 target. Because in AbbVie's expectation, if Rova-T can finally be launched, it will become a blockbuster with a peak sales of $5 billion.
On November 13 last year, Novartis announced the introduction of Legend Biotech's CAR-T therapy LB2102 targeting DLL3. Although LB2102 is still in the preclinical stage, the total transaction amount exceeded $1 billion, and the down payment alone reached $100 million, which is enough to reflect Novartis' high expectations for the DLL3 target. Today, with the positive clinical data readout, ZL-1310 has also attracted the attention of multiple investment banks. Jefferies analysts believe that Tarlatamab's peak sales are expected to be about $1.5 billion to $2 billion, and ZL-1310 has a differentiated advantage, so the peak sales are expected to reach $3 billion.
It is foreseeable that, driven by ZL-1310, the popularity of the DLL3 target will further increase. Of course, for global pharmaceutical companies, they need to rely on technology to win. Rova-T's two phase 3 clinical trials unfortunately failed, giving way to the new generation of DLL3 ADC. ZL-1310 is the leader in the challenge team. It uses a topoisomerase 1 inhibitor as a payload, which is more toxic, but uses a tumor-specific release linker, which can be released both in the tumor microenvironment and in tumor cells, so it can achieve "reduced toxicity and increased efficacy". All innovative drug research and development is a process of groping for the optimal solution, and there is no end to this road. In the future, in the field of DLL3 targets, only players who find the optimal solution can stand out. With the sounding of the SCLC battle horn, we look forward to more domestic players seizing the opportunity in the future.
https://mp.weixin.qq.com/
By editorRead more on
- Gan & Lee Pharmaceuticals’ new PROTAC drug GLR2037 tablets have been approved for clinical trials to enter the field of prostate cancer treatment March 3, 2026
- AideaPharmaceuticals plans to raise no more than 1.277 billion yuan through a private placement to focus on the global clinical development of innovative HIV drugs March 3, 2026
- Giant Exits! Its Star Business Acquired March 3, 2026
- Focusing on cardiovascular and cerebrovascular diseases! OpenMediLead Medical Intelligence Dual Engines Launch Internal Testing, Connecting Drug Development and Clinical Diagnosis in a Closed Loop March 3, 2026
- Innovent Biologics Announces Approval of New Indication for BTK Inhibitor “Pitubrutinib” in China March 3, 2026
your submission has already been received.
OK
Subscribe
Please enter a valid Email address!
Submit
The most relevant industry news & insight will be sent to you every two weeks.



