Real-World Study Confirms Lower Brain Bleed Risk with Dabigatran
November 14, 2017
Source: medpagetoday
 951
951
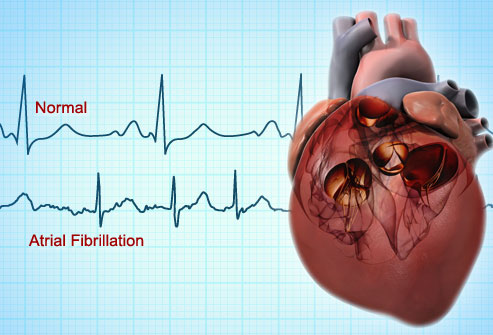
Real-world outcomes among patients with atrial fibrillation taking the anticoagulant dabigatran (Pradaxa) mimic those reported in clinical trials, with dabigatran use associated with lower rates of brain bleeds, and similar rates of stroke and extracranial hemorrhage as treatment with warfarin in a new study.
Researchers examined data from the Sentinel Initiative, which is a national electronic prescription-drug surveillance system established by the FDA to monitor the safety of newly approved drugs and medical products.
Dabigatran was approved by the FDA in 2010 to reduce stroke risk in patients with nonvalvular Afib, based on findings from the RE-LY clinical trial.
The new study, published Monday in Annals of Internal Medicine, compared stroke, bleeding and myocardial infarction rates in patients treated with dabigatran versus warfarin in more than 55,000 patients treated in clinical practices across the United States since the drug was approved.
"Our findings suggest that results from the trial do appear to translate pretty well into clinical practice in terms of similar rates of ischemic stroke compared to warfarin and (overall) bleeding and lower rates of brain bleeds," lead author Alan S. Go, MD, of Kaiser Permanente Northern California told MedPage Today.
As with the RE-LY data, there was a slightly higher rate of myocardial infarctions associated with dabigatran use in the study, but the association was not seen in all statistical analyses performed by the researchers. Subgroup analyses showed the association in men, but not women, and in older Afib patients.
"In the original trial used for FDA approval, they did notice more heart attacks in patients taking dabigatran, but this did not meet statistical significance," Go said. "We also saw a higher rate in clinical practice, but, depending on how we analyzed the data, it wasn't always statistically significant."
He added that more research is needed to better understand this observed association.
The retrospective cohort study included adults with Afib initiating dabigatran or warfarin therapy between November of 2010 and May 2014 within the Sentinel Initiative network, which includes a central coordinating center and 17 collaborating institutions and health care delivery systems.
The study included 25,289 patients starting dabigatran therapy and 25,289 propensity score-matched patients starting warfarin therapy.
The analysis revealed that:
- Dabigatran- and warfarin-treated patients did not have significantly different rates of ischemic stroke (0.80 versus 94 events per 100 person-years, HR 0.92; 95% CI 0.65-1.28)
- Similar rates of extracranial hemorrhage were also seen for the two drugs (2.12 versus 2.63 events per 100 person-years, HR 0.89; 95% CI 0.72-1.09)
- Dabigatran treatment was associated with a lower rate of intracranial bleeding (0.39 versus 0.77 events per 100 person-years, HR 0.51; 95% CI 0.33-0.79)
- Dabigatran treatment was associated with a higher rate of MI (0.77 versus 0.43 events per 100 person-years, HR 1.88; 95% CI 1.22-2.90)
"However, the strength and significance of the association between dabigatran use and myocardial infarction varied in sensitivity analyses and by exposure definition," the researchers wrote.
Gastrointestinal bleeding risk was also higher in older patient treated with dabigatran and in dabigatran-treated patients with kidney dysfunction.
Go said the main strength of the analysis was the use of the FDA surveillance system data, given that previous clinical practice studies have been largely limited to Medicare data.
"This provides a much more representative look across the age spectrum of patients with atrial fibrillation," he said.
Study limitations included the lack of information on outpatient international normalized ratios for most warfarin-treated patients, which limited the researchers' ability to characterize longitudinal exposure and quality of anticoagulation.
All the patients included in the study had health insurance, and the researchers warned that the findings may not be generalizable to uninsured patients.
Also, as in earlier studies, the duration of continuous exposure to dabigatran or warfarin was relatively short and drug adherence could not be directly measured.
By DduRead more on
- Things to Know before Buying Newborn Baby Incubators March 31, 2022
- US approves Pradaxa as oral blood thinning med for children June 23, 2021
- AZ’s Farxiga Gets FDA Priority Review For Heart Failure January 8, 2020
- Highly Resistant Food Poisoning Bug Responds to Antibiotics September 6, 2018
- Smartphone Based Diagnosis to Identify Mosquitoes Transmitting Infection September 5, 2018
your submission has already been received.
OK
Subscribe
Please enter a valid Email address!
Submit
The most relevant industry news & insight will be sent to you every two weeks.



