FDA Awards Accelerated Approval to Gilead Sciences Drug for Rare Liver Disease
August 16, 2024
Source: drugdu
 402
402
Livdelzi is now FDA-approved for treating the rare liver disease primary biliary cholangitis. Gilead Sciences added the drug to its pipeline via the $4.3 billion acquisition of CymaBay Therapeutics earlier this year.
By Frank Vinluan 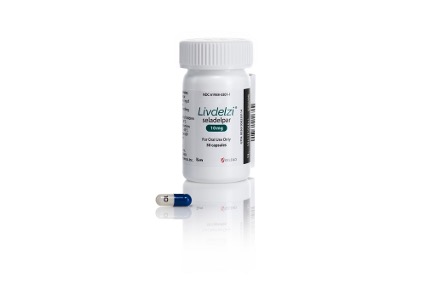 A Gilead Sciences drug acquired earlier this year in a multi-billion dollar deal is now FDA approved as new treatment for primary biliary cholangitis (PBC), a rare liver disease that can lead to liver failure.
A Gilead Sciences drug acquired earlier this year in a multi-billion dollar deal is now FDA approved as new treatment for primary biliary cholangitis (PBC), a rare liver disease that can lead to liver failure.
The approval announced Wednesday for the drug covers the treatment of adults whose disease is inadequately managed by the standard of care PBC drug as well as those who cannot tolerate that drug. The Gilead therapy, seladelpaar, will be marketed under the brand name Livdelzi.
PBC is a rare, progressive autoimmune condition that leads to inflammation and scarring of the liver’s bile ducts. The chronic disorder, which impairs liver function, mainly strikes women over 40 years of age. Gilead estimates that 130,000 people in the U.S. have this rare disease. The first line of treatment is ursodiol, an old gallstone drug that went on to receive an additional approval for PBC. Ocaliva, a drug developed by Intercept Pharmaceuticals (now part of Alfasigma), won FDA approval in 2016 as a second-line PBC treatment. This once daily pill reduces bile production, preventing it from building up and damaging the liver.
Livdelzi is a small molecule designed to bind to and activate peroxisome proliferator activated receptor delta (PPAR delta). This receptor regulates several metabolic processes, but the way Livdelzi works to treat PBC is not fully understood. Published research for the drug indicate that activating PPAR delta reduces bile acids by downregulating the enzyme key to synthesizing bile acids from cholesterol.
Livdelzi, a once-daily capsule, was evaluated in a placebo-controlled Phase 3 study that enrolled 193 participants, most of whom received the study drug alongside standard of care ursodiol. The main goal was a composite measure of biochemical response. Results showed 62% of participants treated with the study drug showed such a response compared to 20% of those who received a placebo.
The key component of the composite biochemical response was measuring for alkaline phosphatase (ALP), an enzyme whose elevated levels indicate liver problems. High ALP is considered a predictor of the risk for liver transplant and death. In the pivotal study, 25% of patients in the Livdelzi group achieved ALP levels in the normal range after 12 months versus zero participants in the placebo arm. Some liver diseases, including PBC, are also associated with pruritus, or severe itching. In the clinical trial, Livdelzi led to a statistically significant reduction in pruritus compared with placebo. Results were published in February in the New England Journal of Medicine.
The FDA decision for the Gilead drug is an accelerated approval based on ALP reduction. That’s the same basis for the accelerated approval of Intercept’s PBC drug. Both drugs have not yet shown they can help PBC patients live longer or prevent a decline in liver function. Those benefits must be verified in confirmatory studies. Gilead said ongoing tests of Livdelzi include a placebo-controlled confirmatory Phase 3 test that will assess the drug’s impact on survival in patients with compensated liver cirrhosis due to PBC.
As Livdelzi enters the market, one key differentiator could be safety. The label for Intercept’s Ocaliva carries a black box warning due to the risk of the loss of liver function or liver failure in patients with compensated or decompensated cirrhosis. While Gilead’s drug is also not recommended for patients with decompensated cirrhosis, its label has no black box warning.
Livdelzi was originally developed by Johnson & Johnson. In 2006, CymaBay Therapeutics licensed the drug and advanced its clinical development. The prevalent fatty liver disease now called metabolic dysfunction-associated steatohepatitis (MASH) was at one time the lead disease indication for the molecule. A safety signal led to an FDA clinical hold in 2019. When that hold was lifted the following year, CymaBay decided to focus on developing the drug for PBC. This past winter, with the PBC drug already under FDA review, Gilead reached a $4.3 billion deal to buy CymaBay. Last month, Gilead paid J&J subsidiary Janssen $320 million to cover any future royalties owed for Livdelzi.
Livdelzi is now part of a broader Gilead liver drug portfolio that includes the hepatitis C treatment Epclusa and hepatitis B products Vemlidy and Viread. A Gilead spokesperson said Livdelzi will be rolled out to pharmacies across the U.S. starting early next week. Pricing information will released in coming days. The Gilead PBC drug is still under regulatory review in Europe.
“People living with PBC have been waiting for treatment advancements for many years,” Gilead Chairman and CEO Daniel O’Day said in a prepared statement. “Today’s approval of Livdelzi, with its distinct profile, provides them with an important new option. We look forward to leveraging Gilead’s long-standing expertise in liver disease to bring this promising new treatment to all those who could benefit.”
Photo: Business Wire
Read more on
- The first subject has been dosed in the Phase I clinical trial of Yuandong Bio’s EP-0210 monoclonal antibody injection. February 10, 2026
- Clinical trial of recombinant herpes zoster ZFA01 adjuvant vaccine (CHO cells) approved February 10, 2026
- Heyu Pharmaceuticals’ FGFR4 inhibitor ipagoglottinib has received Fast Track designation from the FDA for the treatment of advanced HCC patients with FGF19 overexpression who have been treated with ICIs and mTKIs. February 10, 2026
- Sanofi’s “Rilzabrutinib” has been recognized as a Breakthrough Therapy in the United States and an Orphan Drug in Japan, and has applied for marketing approval in China. February 10, 2026
- Domestically developed blockbuster ADC approved for new indication February 10, 2026
your submission has already been received.
OK
Subscribe
Please enter a valid Email address!
Submit
The most relevant industry news & insight will be sent to you every two weeks.



