Is Parkinson’s a Military Base’s Toxic Legacy?
May 19, 2023
Source: drugdu
 318
318
F. Perry Wilson, MD, MSCE
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I'm Dr F. Perry Wilson of the Yale School of Medicine.
The thing to realize about this story is that even if it were just a problem for the military, it would be a huge problem. But although this is a story about the military, in the end, it may affect a much larger segment of the population. It's a story about a military base, Camp Lejeune, and the toxins that leached into the water system there, poisoning the base residents for decades.
It is about the most rapidly growing neurologic disease in the country. And it is very much about a simple molecule, trichloroethylene (TCE). TCE was first synthesized in 1864 and quickly became a sensation as an early anesthetic. Less toxic to the liver than chloroform, and less volatile than highly flammable ether, the substance was used routinely for nearly 100 years until halothane hit the market as a superior anesthetic.
But TCE remained useful in multiple industries, thanks to the fact that it was a powerful organic solvent; it could be used to extract vegetable oils from plants, caffeine from coffee, and for dry cleaning. By the 1970s, however, the dark side of TCE was becoming better understood. Exposure led to fetal malformations, and its use has been linked to a slew of cancers.
But I told you that this is a story about a neurologic disease. And it is.
Expose a mouse to TCE and neurons in the substantia nigra of its brain start to deteriorate. This is the very area that is affected in human Parkinson's disease. But until now, it wasn't entirely clear whether TCE exposure could cause Parkinson's disease in humans.
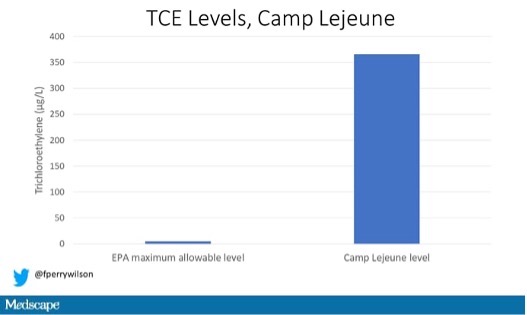
The groundwater at Camp Lejeune, in Jacksonville, North Carolina, was extensively contaminated with TCE from 1953 to 1987. The Environmental Protection Agency (EPA) sets the allowable level of TCE in drinking water at 5 µg/L. The water that servicemen and -women at Camp Lejeune drank, washed, and cooked with had levels of 366 µg/L — more than 70 times higher.
Exposure for individual servicemembers was limited a bit by the time spent on the base, a median of 25 months. Would that be enough to lead to Parkinson's disease in the future?
Researchers led by Samuel Goldman at the Veterans Affairs (VA) Medical Center in San Francisco performed the analysis, appearing in JAMA Neurology.
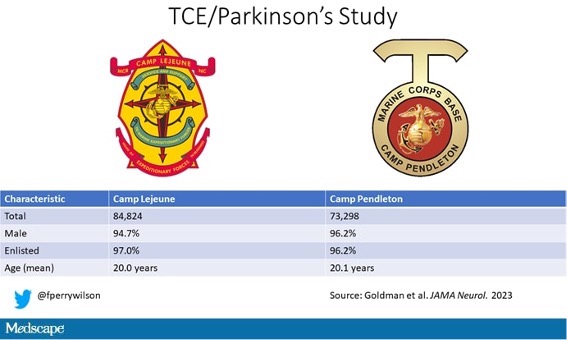
They identified 84,824 individuals who spent more than 3 months at Camp Lejeune during the contamination period and received follow-up care at the VA over the next four to five decades. As a control group, they identified 73,298 individuals who spent that time at Camp Pendleton in California. Not surprisingly, these groups were predominantly male and mostly enlisted men and women. They were young as well — just 20 years old or so when they were spending time at the camps.
Diagnoses of Parkinson's disease were initially made by diagnosis codes and then validated by direct examination of medical records. In that way, 279 cases of Parkinson's disease were found among those who were at Camp Lejeune, and 151 at Camp Pendleton. After adjustment for age, sex, race, and ethnicity, that translated to a 70% higher risk for Parkinson's disease for those who trained at Camp Lejeune compared with Camp Pendleton — a fairly damning result.
But I can't really discuss this study without talking about the problem of detection bias. Detection bias is what occurs when you look harder for something in one group than another, leading to the illusion that it is more common in that group, when in reality you just missed cases in the other group.
In 2017, the VA added service at Camp Lejeune to its list of service-connected conditions, making those from Camp Lejeune eligible for VA healthcare. This speaks to the VA's knowledge that long-term adverse events may occur in these servicemembers, and there is certainly the possibility that doctors would be on the lookout for neurologic conditions.
Excluding those diagnosed after 2017 substantially diminished the association between service at Camp Lejeune and Parkinson's disease, suggesting that some detection bias might be at play. That said, if detection bias were the sole reason for the finding, you'd expect to see higher rates of other neurologic conditions in those from Camp Lejeune as well, but there was no difference in the rates of progressive supranuclear palsy, corticobasal degeneration, or multiple system atrophy.
Parkinson's disease, fortunately, is rare, affecting about 1 in 500 adults in the US. But that still translates to 1 million people in this country living with the condition, and the rate is increasing. TCE exposure may not be rare, with the EPA noting that up to 18% of drinking water samples in the US test over the limit for TCE. Ray Dorsey, a leading Parkinson's disease researcher, says Parkinson's is largely a human-made disease, caused by exposure to toxins and pollutants, and as such, it is a disease that can be ended by us as well. Should this manuscript motivate the powers-that-be to take real action on environmental toxins, I suppose we will have one more reason to thank these brave men and women for their service.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale's Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here on Medscape. He tweets @fperrywilson and his new book, How Medicine Works and When It Doesn't, is available now.
Read more on
- The first subject has been dosed in the Phase I clinical trial of Yuandong Bio’s EP-0210 monoclonal antibody injection. February 10, 2026
- Clinical trial of recombinant herpes zoster ZFA01 adjuvant vaccine (CHO cells) approved February 10, 2026
- Heyu Pharmaceuticals’ FGFR4 inhibitor ipagoglottinib has received Fast Track designation from the FDA for the treatment of advanced HCC patients with FGF19 overexpression who have been treated with ICIs and mTKIs. February 10, 2026
- Sanofi’s “Rilzabrutinib” has been recognized as a Breakthrough Therapy in the United States and an Orphan Drug in Japan, and has applied for marketing approval in China. February 10, 2026
- Domestically developed blockbuster ADC approved for new indication February 10, 2026
your submission has already been received.
OK
Subscribe
Please enter a valid Email address!
Submit
The most relevant industry news & insight will be sent to you every two weeks.



