Laser speckle imaging can identify hearts suitable for transplantation
April 27, 2023
Source: drugdu
 469
469
In the majority of cases, graft failure after heart transplantation is attributable to abnormalities like severe coronary artery disease. As donors with extended criteria like advanced age and pre-existing heart conditions become eligible for heart transplantation, careful screening for congenital abnormalities has become crucial. Invasive coronary angiography is an essential screening tool that can detect coronary artery disease (CAD), a condition characterized by cholesterol deposits in the heart's arteries. However, logistical challenges limit utility so it's used for fewer than a third of donors who are at risk of developing CAD.
To overcome this limitation, a new heart preservation procedure called "ex situ heart perfusion" (ESHP) has been developed. By allowing the supply of oxygenated nutrients to the heart via blood vessels, ESHP allows doctors to monitor the performance of the heart and screen it for any defects outside the body. However, coronary angiography conducted during ESHP is known to damage the heart and result in primary graft failure. Alternative coronary imaging tools are therefore required to identify abnormal blood flows in donor hearts and to determine their eligibility for transplantation.
As reported in the Journal of Biomedical Optics (JBO), a team of researchers led by Professor Elise Colin from Paris Saclay University, France, has introduced a safe and non-invasive optical technique that allows imaging of coronary blood circulation in donor hearts during ESHP. The method utilizes a recently developed speckle imaging technique, known as Laser Speckle Orthogonal Contrast Imaging (LSOCI), that was developed to detect the multiple scattering of moving red blood cells.
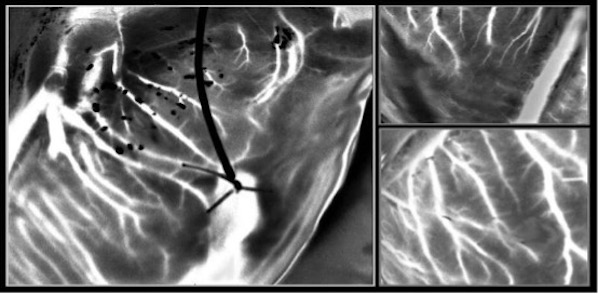
In this study, the researchers improved the imaging capability of LSOCI to observe small blood vessels in the heart. The proposed method thus analyzes blood flow in the heart using a specific polarimetric filtering process that allows suppression of surface scattering. Thus, the time varying speckle patterns used for the imaging process are mainly generated by multiple scattering on moving red blood cells inside peripheral vessels.
"The optical technique allows high-resolution imaging of the entire peripheral vasculature of the heart in real time," says Colin.
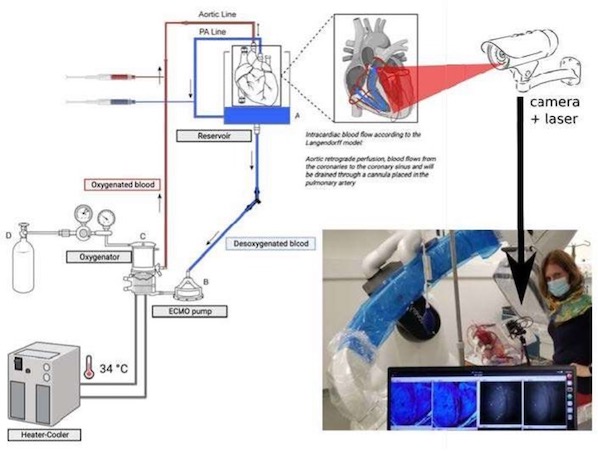
To test this method, the researchers developed a clinical model to study coronary circulation on donor hearts before transplantation. They then used a laser and a camera mounted on an articulated arm fixed above the perfusion module—which contained the donor heart—to generate and analyze rapidly varying speckle patterns.
To overcome the challenges in tracking vasculature due to the beating of the heart, the researchers further optimized the technique with a method called Multi-Period-Enhanced Signal-to-Noise Ratio (MPE-SNR). They took a series of images over time to build a set of frames that depicted the vasculature at similar heart positions. Each image in this sequence was then optimized using the other images to reduce noise and enhance details. The optimized image represented the vasculature at a different time point, and the researchers used a sequence of such images to visualize vasculatures as small as 100 microns in a few seconds.
The newly developed imaging technique enables precise visualization of blood circulation. In the future, this technique can potentially identify myocardial perfusion abnormalities that indicate underlying heart conditions, such as coronary artery disease.
According to Amy Oldenburg, Professor at the University of North Carolina at Chapel Hill and JBO Associate Editor, "The non-contact technique, based on laser speckle, provides imaging of blood circulation within donor hearts and has important implications for identifying hearts that are safe and suitable for transplantation."
Journal information: Journal of Biomedical Optics
By editorRead more on
- 20-Valent Pneumococcal Vaccine Approved for Clinical Trials January 20, 2026
- ADC205 Tablets Received Approval for Drug Clinical Trial January 20, 2026
- Sifang Optoelectronics makes strategic investment in Changhe Biotechnology January 20, 2026
- Mingde Bio plans to acquire a 51% stake in Hunan Lanyi through capital increase and acquisition January 20, 2026
- accelerating the transition of CLL treatment into a “chemotherapy-free era”. January 20, 2026
your submission has already been received.
OK
Subscribe
Please enter a valid Email address!
Submit
The most relevant industry news & insight will be sent to you every two weeks.



